If you are getting pain in the hip or the groin limiting your activity, or disturbing your sleep you may have hip arthritis. Maybe your doctor has already diagnosed you, or you know a friend or relative who has suffered with a bad hip. If this is the case you might need a hip replacement.
Total Hip Replacement Surgery
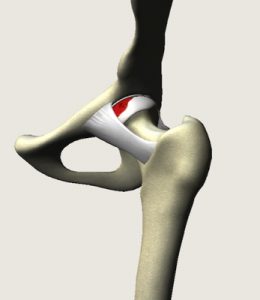
Your hip is a ball and socket joint lined with articular cartilage. If your cartilage is worn out or damaged it can make your joint painful and stiff, and the joint becomes inflamed. This is arthritis, and when the pain becomes too much the best treatment can be a joint replacement.
A hip replacement usually improves mobility and reduces pain, although your new hip may not be able to bend quite as far as a good normal hip joint, it will likely be much better than your arthritic hip. One of the most troublesome aspects of hip arthritis is
disturbed sleep. If your walking is severely limited, you are inconstant pain, and your sleep is disturbed then you are likely to benefit from a hip replacement. Surgery is usually recommended only if non-surgical treatments, such as physiotherapy and exercise, taking medicines or using physical aids like a walking stick, no longer help to reduce pain or improve mobility.
Types of artificial hip
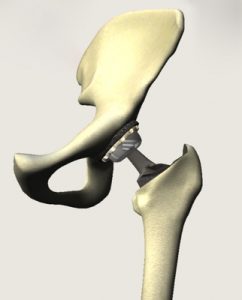
Artificial hip parts can be made of metal, ceramic or plastic. Hip joints can be fixed in place using a special substance called ‘bone cement’. Alternatively, they may be designed so that your own bone grows onto the metal. These ‘uncemented’ hips can be coated with a type of bone mineral (hydroxyapatite) or can be made from a material that has lots of tiny holes (porous coating). This encourages your bone to grow into the artificial joint and fix it in place. Dr. Amit prefers to use a cemented hip replacement, and tailors the choice of bearing surface to your needs. He does not use metal on metal bearings which have caused a lot of problems recently. Hip replacements usually last from 10 to 20 years, after which they need replacing with a “revision hip replacement”.
What are the alternatives to hip replacement?
Surgery is usually recommended only if non-surgical treatments, such as taking painkillers (e.g. paracetamol) or anti-inflammatories (e.g. ibuprofen), or using physical aids like a walking stick, no longer help to reduce your pain or improve mobility. Sometimes a steroid injection into the hip can help to establish that the pain is coming from the hip joint itself, and this can be useful in postponing the need for a hip replacement for many months.
Preparing for your operation
Dr. Amit will explain how to prepare for your operation. For example if you smoke you will be asked to stop, as smoking increases your risk of getting a chest and wound infection, which can slow your recovery. Losing excess weight can be very beneficial before a hip replacement. It makes the surgery easier and safer, and makes the hip replacement last longer. Many people think they will lose weight after their hip replacement, but scientific studies show that this does not usually happen.
The operation usually requires a hospital stay of a few days and it’s done under spinal anaesthesia and sedation. This means you will be asleep during the operation and the bottom half of the body will be numbed. By avoiding general anesthesia your recovery will be faster and you will typically be sitting out in a chair or walking within hours. You can have a general anesthetic if you prefer, but this does slow your recovery. Either way you will be asked to follow fasting instructions. This means not eating or drinking, typically for about six hours before a general anaesthetic. However, it’s important to follow your anaesthetist’s advice.
At the hospital, your nurse will check your heart rate and blood pressure, and test your urine.
Dr. Amit will discuss with you what will happen before, during and after your procedure, and any pain you might have. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, which you will be asked to do by signing a consent form.
You will be given compression stocking on the both legs to help prevent blood clots forming in your veins (deep vein thrombosis, DVT). You will also need to have an injection of an anticoagulant medicine as well as stockings.
About the operation
A hip replacement usually takes around two hours.
Your surgeon will make an incision over your hip on the side. He will then separate the ball and socket (hip joint).
The ball at the top end of your thigh bone (the femoral head) will be removed and a replacement ball on a stem will be inserted into your thigh bone. Your hip socket will be hollowed out to make a shallow cup and an artificial socket will be placed into it. The two halves of the hip joint are then put back together (the ball is put into the socket). He will close the skin cut with stitches or clips and cover it with a dressing.
What to expect afterwards
You will need to rest until the effects of the anaesthetic have passed. You may not be able to feel or move your legs for several hours after a spinal anaesthetic.
You may need pain relief to help with any discomfort as the anaesthetic wears off, and will be given strong pain killers.
You will have compression stockings on both legs. This helps to maintain circulation. You will be given anticoagulants to reduce the risk of blood clots.
The compression dressing on the hip will be taken down at 48 hours. The adhesive dressing underneath will appear bloodstained and dirty, but it has been put on in a sterile environment, so it will usually be kept in place for 2 weeks. At the 2 week stage the dressing will be removed along with the clips or stitches and the wound should be healed.
A physiotherapist will usually guide you daily through exercises to help your recovery. You will be in hospital until you can walk safely with the aid of sticks or crutches. When you’re ready to go home, you will need to arrange for someone to drive you.
Your nurse will give you some advice about caring for your hip and a date for a follow-up appointment before you go home. This will usually be for 2 weeks to take the stitches out.
You will stay in hospital until you’re able to walk safely with the aid of sticks or crutches. This is usually a few days. However, if you’re generally fit and well, Dr. Amit uses an accelerated rehabilitation programme, where you start walking on the day of the operation and are discharged within three to five days.
Recovering from hip replacement surgery
You will be provided with pain killers after your surgery. Only take them if you need them. Despite our best efforts this surgery can be painful. Many patients find that in hospital with the support of the nurses and physios that they cope quite well, but that the first few days at home can be tough. Be prepared for this, and make sure that your relatives or friends can be there to support you.
The physiotherapy exercises are a crucial part of your recovery, so it’s essential that you continue to do them for at least two months.
There are certain movements that you shouldn’t do in the first six weeks. For example, don’t cross your legs or twist your hip inwards and outwards. This is to reduce strain on your scar and to reduce the risk of a dislocation. Your physiotherapist will give you further advice and tips to protect your hip.
You should be able to move around your home and manage stairs. You will find some routine daily activities, such as shopping, difficult for a few weeks and will need to ask for help. You will need to use crutches for about four to six weeks.
You can usually return to light work after about six weeks. But if your work involves a lot of standing or lifting, you may need to stay off for longer.
You need to wear your compression stockings for six weeks.
You shouldn’t drive until you are confident that you could perform an emergency stop without discomfort. Typically this is 6 weeks.
What are the risks?
Hip replacement surgery is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure. Overall about 98% of the time things go smoothly. The risks and complications are as follows:
Rare:
- Anaesthetic problems
- Infection – this can be a disaster needing months of intravenous antibiotics, possibly changing the hip implant. Antibiotics are given after the surgery to prevent this
- Bleeding – rarely needing a blood transfusion
- Scar down the side of the hip
- Blood clots (DVT or PE) anticoagulants are given after the surgery to prevent this
- Wearing out or working loose over the years needing more surgery
- Dislocation, this can need an anesthetic to put the hip back in joint, and sometimes need revision hip surgery if it happens again
- Problems with the leg length, sometimes needing a shoe raise
- Fracture of the bone around the implant
- Stiffness, this is usually treated with intensive physio and hydrotherapy
Really rare but really serious:
- Damage to an important blood vessel or nerve – this is very rare but can be very serious
- Death! Every year somewhere in the world patients die during or soon after their joint replacement surgery. Because you will have been thoroughly checked before the surgery people who have had joint replacements actually have a lower risk of dying that those who have not
Dr. Amit will discuss these with you prior to surgery. If you have any questions it may be helpful to note them down to remind you to ask him.
