If you have bad knee arthritis knee replacement may be the answer
If you are getting long-term pain in the knee, with stiffness and difficulty getting around you may well have knee arthritis. Maybe your doctor has already told you that you have arthritis, or you know friends or relatives that have been through it. If you have knee arthritis then you may well need to have a knee replacement. If you are not sure Dr. Amit to talk it through.
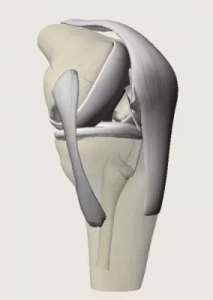
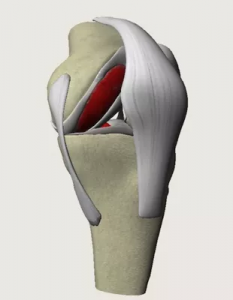
Your knee joint is made up by the ends of your thigh bone (femur) and shin bone (tibia). These normally glide over each other easily because they are covered by smooth articular cartilage. If your cartilage is worn out or damaged it can make your joint painful and stiff, and the joint becomes inflamed. This is arthritis, and when the pain becomes too much the best treatment can be a joint replacement.
A knee replacement usually improves mobility and reduces pain, although your new knee will not be able to bend quite as far as a good normal knee joint, it will likely be much better than your arthritic knee.
One of the most troublesome aspects of knee arthritis is disturbed sleep. If your walking is severely limited, you are in constant pain, and your sleep is disturbed then you are likely to benefit from a knee replacement. Surgery is usually recommended only if non-surgical treatments, such as physiotherapy and exercise, taking medicines or using physical aids like a walking stick, no longer help to reduce pain or improve mobility.
Depending on the condition of your knee joint, you may have part or all of your knee joint replaced. A total knee replacement is more common, but if your knee is suitable for a partial knee replacement you will enjoy better function.

Types of Knee replacement
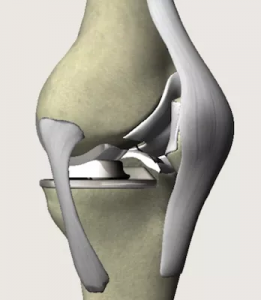
Replacement knee parts are made of a special metal alloy called cobalt chrome and special plastic called ultra high molecular weight polyethylene. A knee replacement can last for over 20 years in the right conditions.
Not all knee replacements are equal! Many of the designs used in the NHS are based on ideas from 40 years ago and are old fashioned, cheap, and are associated with quite high levels of dissatisfaction. Dr. Amit is very interested in ‘High-Performance Knee Replacement’.
There are also a variety of knee replacements called ‘Partial knee replacements’ also known as ‘unicompartmental knee replacement’ or ‘Oxford knee replacement’. These can be used when only one of the three parts of the knee is damaged and the remaining two are healthy. We now know that on average partial knee replacements, function better, but do not last as long as total knee replacements. It is a smaller operation, which smaller risks and better function. Also when the remainder of the knee does wear out it is easier to change than a full knee replacement. The decision between the two is something that you should give careful thought over, and discuss with Dr. Amit.
Preparing for a knee replacement
Dr. Amit will explain how to prepare for your operation. For example, if you smoke you will be asked to stop, as smoking increases your risk of getting a chest and wound infection, which can slow your recovery. Losing excess weight can be very beneficial before a knee replacement. It makes the surgery easier and safer and makes the knee replacement last longer. Many people think they will lose weight after their knee replacement, but scientific studies show that this does not usually happen.
The operation usually requires a hospital stay of a few days and it’s done under spinal anaesthesia and sedation. This means you will be asleep during the operation and the bottom half of the body will be numbed. By avoiding general anaesthesia your recovery will be faster and you will typically be sitting out in a chair or walking within hours. You can have a general anaesthetic if you prefer, but this does slow your recovery. Either way, you will be asked to follow fasting instructions. This means not eating or drinking, typically for about six hours before a general anaesthetic.
At the hospital, your nurse will check your heart rate and blood pressure, and test your urine. If there is any sign that you have an active infection (e.g. an infected toenail, or a urine infection) your surgery will need to be postponed until this is better.
Dr. Amit will discuss with you what will happen before, during and after your procedure, and any pain you might have. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, which you will be asked to do by signing a consent form.
You will be given compression stocking on both legs to help prevent blood clots forming in your veins (deep vein thrombosis, DVT). You will also need to have an injection of an anticoagulant medicine as well as stockings. The injections need to be given every day for 14 days. The stockings should ideally be worn for 6 weeks.
What happens during a knee replacement?
A knee replacement usually takes around one hour.

Total knee replacement
Dr. Amit will make a single incision down the front of your knee. He will remove the worn or damaged surfaces from both the end of your thigh bone (femur) and the top of your shin bone (tibia). He will shape the surfaces of your thigh and shin bones to fit the artificial knee joint and then fit the new joint over both bones fixing it in place with a special sort of bone cement.
Rarely the back of your kneecap is replaced with a plastic part. This is called patellar resurfacing. Even in the 21st century we still don’t know whether this helps with kneecap pain, hence Dr. Amit usually does not resurface the patella.
The wound will be closed with stitches or clips and covered with a dressing. Dr. Amit will tightly bandage your knee to help minimise swelling.
What to expect afterwards

You will need to rest until the effects of the anaesthetic have passed. You may not be able to feel or move your legs for several hours after a spinal anaesthetic.
You may need pain relief to help with any discomfort as the anaesthetic wears off, and may be given strong painkillers.
You will have compression stockings on both legs. This helps to maintain circulation. You will be given anticoagulants to reduce the risk of blood clots.
The large bandage around the knee will be taken down at 48 hours. The adhesive dressing underneath will appear bloodstained and dirty, but it has been put on in a sterile environment, so it will usually be kept in place for 2 weeks. At the 2 week stage, the dressing will be removed along with the clips or stitches and the wound should be healed.
A physiotherapist will usually guide you daily through exercises to help your recovery. A machine called a CPM machine may be used to help get the knee moving.
You will be in the hospital until you can walk safely with the aid of sticks or crutches. When you’re ready to go home, you will need to arrange for someone to drive you.
Your nurse will give you some advice about caring for your knee and a date for a follow-up appointment before you go home. This will usually be for 2 weeks to take the clips out.
Recovering from knee replacement surgery
You will be provided with painkillers after your surgery. Only take them if you need them. Ice packs and elevation are also helpful. Many patients find that in the hospital with the support of the nurses and physios that they cope quite well, but that the first few days at home can be tough. Be prepared for this, and make sure that your relatives or friends can be there to support you.
The physiotherapy exercises are a crucial part of your recovery, so it’s essential that you continue to do them for at least two months.
You will be able to move around your home and manage stairs. You will find some routine daily activities, such as shopping, difficult for a few weeks. You may need to use a walking stick or crutches for up to six weeks.
You need to wear your compression stockings for six weeks.
When you’re resting, raise your leg and support your knee to help prevent swelling in your leg and ankle.
Depending on the type of work you do, you can usually return to work after 6 to 12 weeks.
You shouldn’t drive until you are confident that you could perform an emergency stop without discomfort. Typically this is 6 weeks.
What are the risks?
Knee replacement surgery is commonly performed and generally very safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure. Overall about 98% of the time things go smoothly. The risks and complications are as follows:
Rare:
- Anaesthetic problems
- Infection – this can be a disaster needing months of intravenous antibiotics, possibly changing the knee implant, or very very rarely can end up in amputation. Antibiotics are given after the surgery to prevent this
- Bleeding – rarely needing a blood transfusion
- Scar down the front of the knee which can have a numb patch around the scar which may take years to improve
- Blood clots (DVT or PE) anticoagulants are given after the surgery to prevent this
- Stiffness, this is usually treated with intensive physio and hydrotherapy, but sometimes needs a manipulation under anaesthesia
- Wearing out or working loose over the years needing more surgery
- Problems with the kneecap, sometimes needing more surgery
Really rare but really serious:
- Damage to an important blood vessel or nerve – this is very rare but can be very serious and very very rarely can lead to amputation
- Death! Every year somewhere in the world patients die during or soon after their joint replacement surgery. Because you will have been thoroughly checked before the surgery people who have had joint replacements actually have a lower risk of dying than those who have not!
